Vacancies in psychiatric positions can have profound implications for healthcare facilities, impacting both financial stability and patient care. These unfilled positions extend beyond immediate staffing challenges and can result in significant losses, operational strain, and deteriorating patient outcomes. In this blog post, we'll explore the financial and operational implications of psychiatrist vacancies and provide strategies to mitigate their effects on healthcare systems.
Financial Implications of Psychiatrist Vacancies
Psychiatrist vacancies can have a serious financial impact on healthcare organizations. A single psychiatrist can generate an average of $1,302,631 in annual revenue—about $108,552 per month. When a position remains vacant for an extended period, the revenue loss quickly adds up. For instance, a six-month vacancy could lead to over $650,000 in lost revenue.
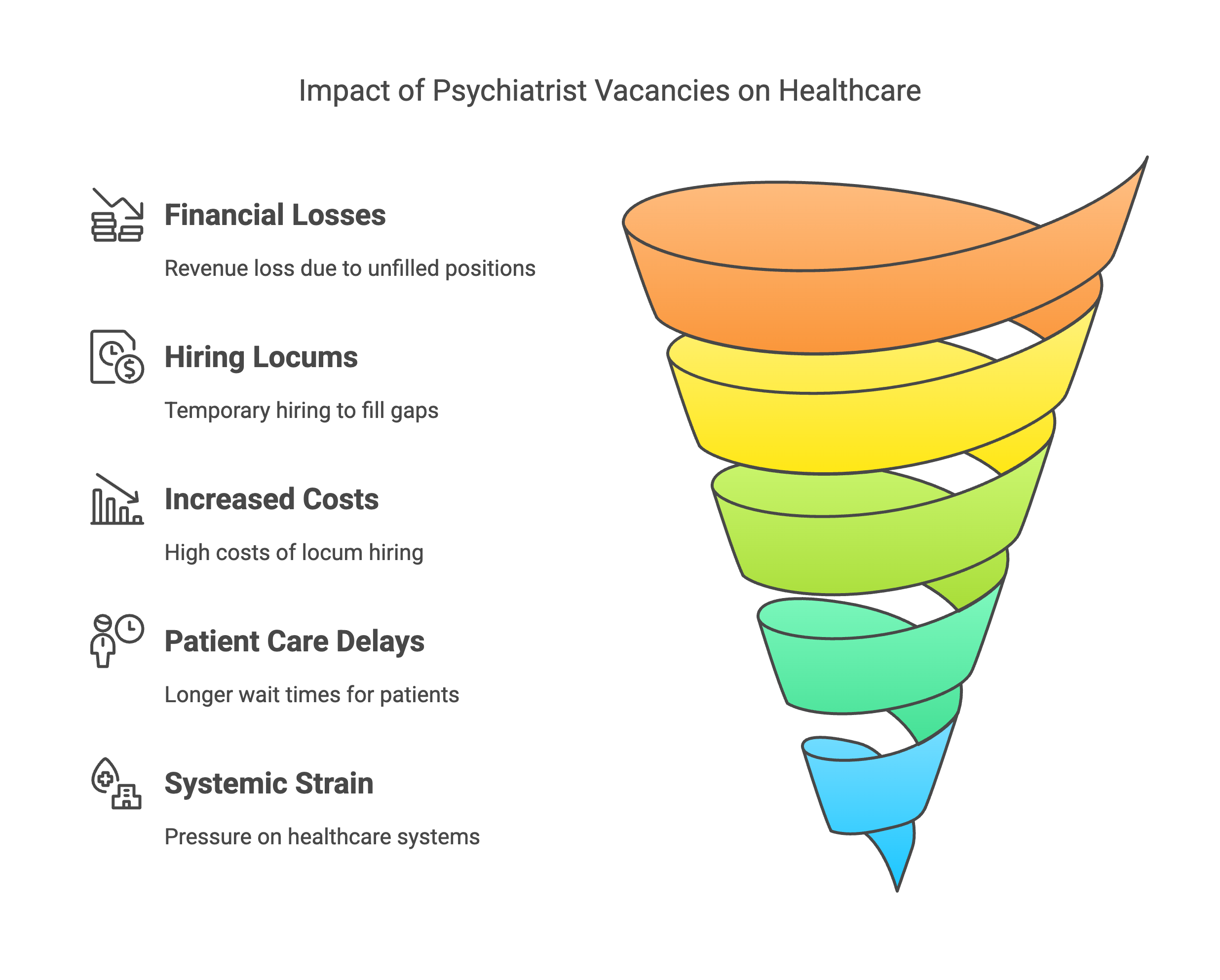
Many healthcare facilities turn to locum tenens psychiatrists—temporary professionals who fill in while a permanent psychiatrist is sought. However, hiring locum psychiatrists can be expensive. In the United States, locum psychiatrists typically earn between $150 to $250 per hour, which can add up to significant costs, especially when vacancies persist over long periods.To help prevent these substantial financial losses, healthcare organizations must focus on strategies that minimize the duration of psychiatrist vacancies and optimize recruitment processes.
Impact on Patient Care and Systemic Strain
While the financial costs are significant, the most urgent concern is the impact psychiatrist vacancies have on patient care. Psychiatrist shortages lead to longer wait times for appointments, overburdened emergency departments, and, in some cases, high-risk patients being turned away. These delays can have severe consequences, including individuals facing self-harm, harm to others, or homelessness due to the lack of timely psychiatric care.
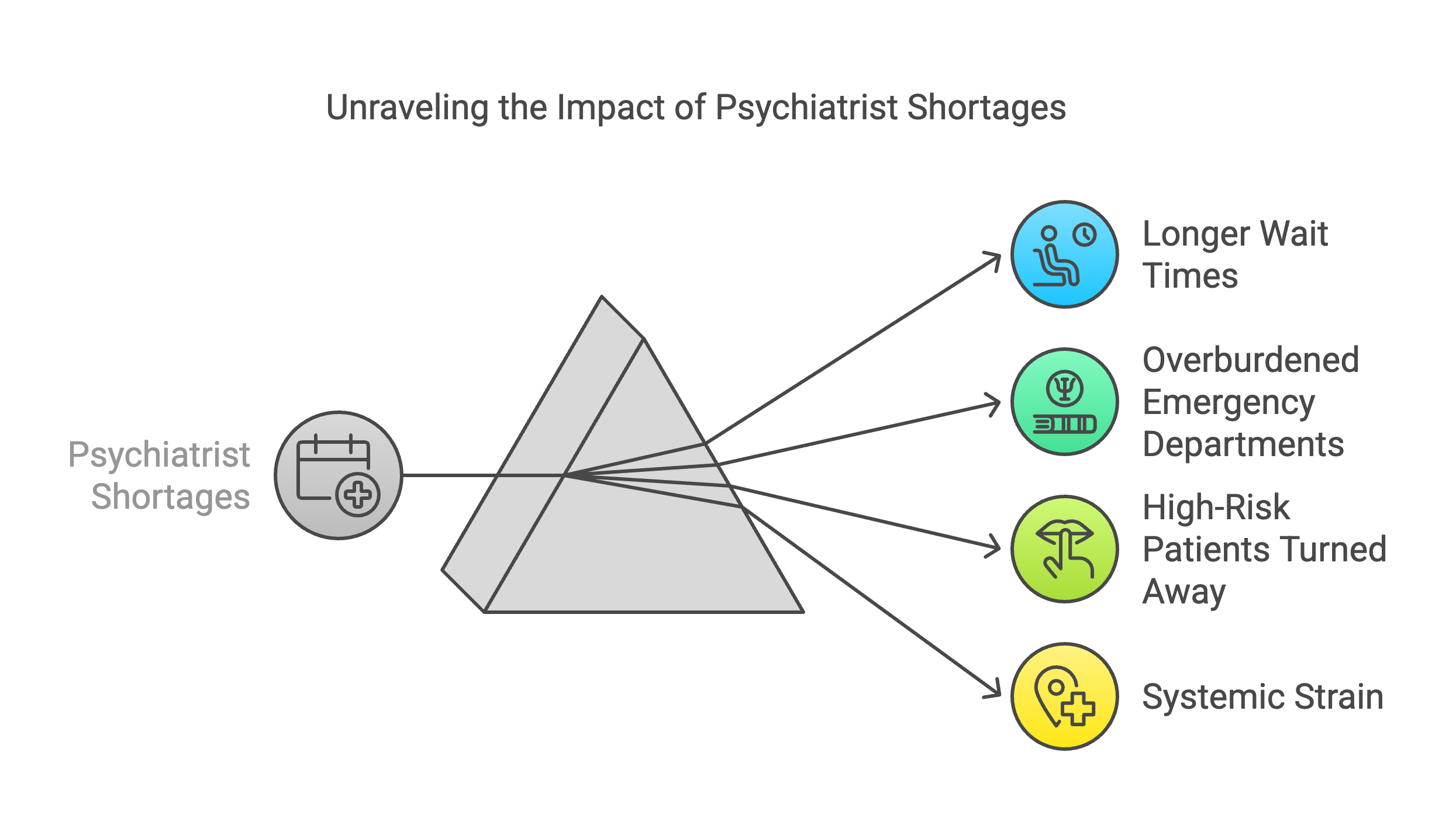
The shortage of psychiatrists also places immense pressure on other parts of the healthcare system. Emergency departments, already under stress, often struggle to manage psychiatric crises, which can increase the overall strain on the healthcare system. This systemic strain further disrupts care and delays treatment, creating a vicious cycle of worsening conditions for patients.
To tackle the challenges posed by psychiatrist vacancies, healthcare facilities can implement several strategies designed to reduce vacancies, improve recruitment efforts, and ensure high-quality patient care.
- Competitive Compensation
Offering competitive compensation packages is one of the most effective strategies for attracting and retaining psychiatrists. In the U.S., research suggests that increasing pay by 25% could result in significant cost savings by reducing reliance on expensive locum tenens staffing. Competitive salaries not only make it easier to fill psychiatrist vacancies but also help healthcare organizations retain skilled professionals. - Retained Search Recruitment
Healthcare organizations can engage in retained search recruitment agreements with specialized staffing firms. These agreements, which involve an upfront fee, lead to more dedicated and efficient recruitment efforts. As a result, healthcare facilities can fill vacancies more quickly, minimizing downtime and reducing the impact on operations. - Investment in Psychiatry Training
Another key strategy is investing in the future workforce. Increasing the number of psychiatry training positions and offering incentives for specialization can help build a strong pipeline of qualified professionals. According to the American Association of Medical Colleges, the U.S. will face a shortage of up to 10,000 psychiatrists by 2030, making it imperative to address training gaps and ensure a sustainable workforce for the future. - Telepsychiatry Solutions
Telepsychiatry is a valuable tool in addressing psychiatrist vacancies, particularly in underserved or rural areas. By implementing telepsychiatry programs, healthcare facilities can expand access to psychiatric services, reduce wait times, and provide timely care even when in-person psychiatrists are unavailable. Telepsychiatry also enables healthcare organizations to address psychiatrist shortages without additional physical infrastructure, making it a cost-effective solution.
Psychiatrist vacancies challenge healthcare systems by causing lost revenue, reduced patient care, and strain on resources. To address this, strategies like competitive compensation, retained search recruitment, psychiatry training, and telepsychiatry can reduce shortages, improve patient outcomes, and enhance efficiency. As demand grows, healthcare facilities must act proactively to fill vacancies, ensuring high-quality care while minimizing financial impact.